Heart disease is the number one cause of death in the United States. And depression is one of the most disabling diseases we face. Heart disease and depression are both widespread among the general population and often can occur simultaneously in the same individual. This relationship is much more than a coincidence. The relationship between heart disease and depression is bidirectional, meaning that each can increase the risk of developing the other. People who are depressed develop heart disease at a higher percentage than the general population and people with no history of depression are at increased risk after a heart attack.
Depression is often the result of several factors:
- A person’s physical health, state of mind, environment and their family history.
- High levels of stress, life transitions, and loss.
- Imbalances in the chemicals that the body uses to control mood.
The link between heart disease, heart attacks and depression
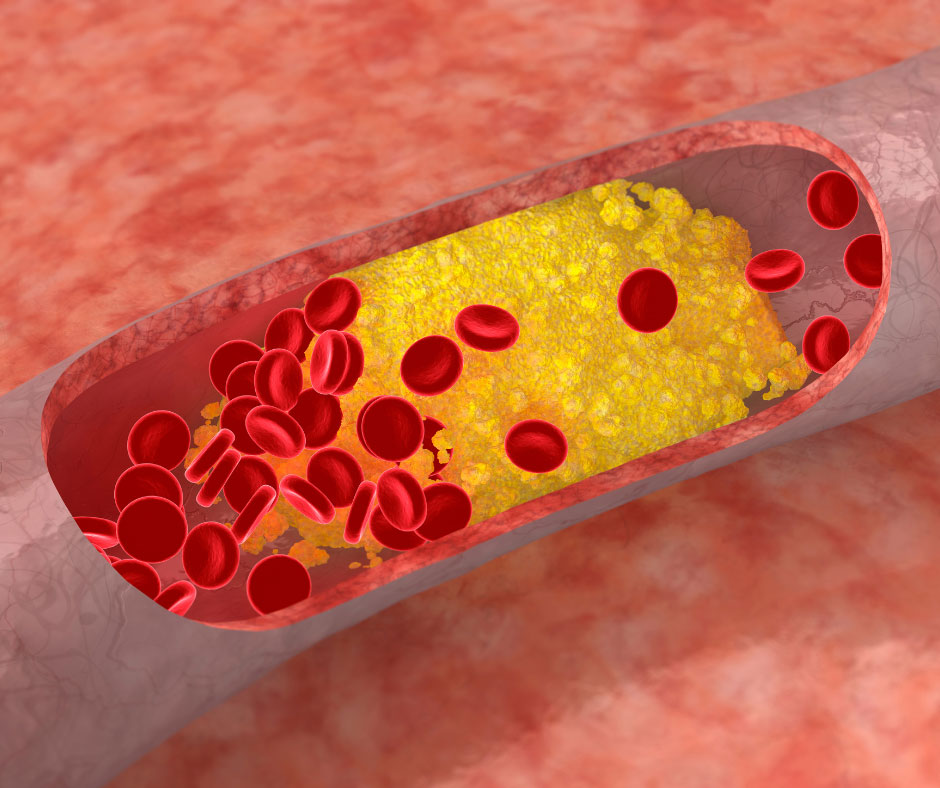
Depression can accelerate the development of heart disease and increase the risk of a heart attack. And conversely, depression is about twice as likely to occur in people who already suffer from heart disease. Plausible explanations for the link between heart disease and depression are poor exercise habits, an unhealthy diet, some medications, and a high usage of smoking, drugs or drinking. These poor lifestyle choices and unmanaged mental stress are risk factors that can lead to blood clots, high blood pressure, irregular heart rhythms, heart attack, low-grade inflammation, and a weakened immune system. “It’s really important for people to be aware of this link and to get treatment for depression, because it can be very debilitating,” says Dr. Christopher Celano, a psychiatrist at the Cardiac Psychiatry Research Program at Harvard-affiliated Massachusetts General Hospital.
Among people who have had a heart attack researchers have estimated the rate of depression is as high as 33%. A heart attack can affect many aspects of a person’s life, including their attitude and mood, confidence in their ability to continue being a productive employee or family member, uncertainty about the future, feelings of guilt and embarrassment, and self-doubt over diminished physical capabilities. These factors can lead to depression, and once depression develops, people lose their desire and energy to follow a recovery regime that includes exercise, healthy eating, refraining from smoking and alcohol and drug use, and taking one’s prescribed medications.
One study found that the risk of death in heart attack survivors with depression was three times greater than those without depression. Depression has been proven to be such a risk factor in cardiac disease that the American Heart Association (AHA) has recommended that all cardiac patients be screened for depression.
Signs of depression
All people have days when they feel sad, gloomy, or down in the dumps, especially after a heart attack or major surgery. But if those feelings last for more than two weeks and you gradually stop feeling hopeful or happy about anything in your life, you may have depression. Sometimes, symptoms of depression can be made worse by certain medications, a physical disorder, or a virus or illness. Signs of depression can include:
- Depressed mood or irritability or tearfulness.
- Excessive fatigue, a lack of energy and trouble concentrating.
- Withdrawal and difficulty with your daily routine, little interest or pleasure in activities, and not responding to family and friends.
- Changes in sleep patterns or appetite.
- Increased negative thoughts and feelings of worthlessness, guilt, despair or loneliness.
- Suicidal thoughts: Suicide is an irreversible solution to problems and causes permanent harm not only to you, but also to family and friends. If you are having thoughts of suicide, call your physician or local 24-hour suicide hotline right away, or go to the nearest emergency room for help.
How is depression diagnosed?
The biggest hurdle to diagnosing and treating depression is recognizing that someone is suffering from it. Unfortunately, approximately half of the people who experience depression are never diagnosed or treated for their illness. Without treatment, depression can become worse. For heart patients, depression can contribute to an increased risk of a heart attack or coronary disease. Not getting treatment can be life-threatening: up to 10 percent of people battling depression commit suicide.
Your health care provider can evaluate your condition by asking you to describe your symptoms, as well as evaluating your personal and family medical history, and any history of drug or alcohol use.
How is depression treated?
When uncertainty and anxiety become debilitating and interfere with the daily functions of life your doctor will likely refer you to a psychotherapist who can provide supportive counseling or “talk therapy”. Psychotherapy can increase a person’s social support, help change patterns in thinking, learn coping skills for symptoms, and help prevent future depressive symptoms. However, finding a good psychotherapist who takes your health insurance and is accepting new patients can be a challenge. Ask your doctor or your health insurance company for referrals. Call several practitioners to get on their waiting lists, and be persistent.
Your health care provider or primary care doctor may also start depression treatment with a safe antidepressant medication (generally a selective serotonin reuptake inhibitor (SSRI) such as sertraline (Zoloft), citalopram (Celexa), or escitalopram (Lexapro).
Many people also find that support groups for heart conditions, mental illness, or both can provide both emotional support and psycho-education. If there isn’t a support group in your area, consider looking online for support.
Individuals recovering from a heart attack or other serious cardiac event can access many types of treatment, including cardiac rehabilitation (structured nutrition and exercise programs), social groups for support and encouragement, and specialized evaluation and treatment by psychologists, psychiatrists, or psychiatric social workers.
Heart disease and depression in women
Depression is generally more common in women than in men, and women with heart disease are more likely to develop depression. Heart disease tends to affect older individuals, and approximately one third of women recovering from a heart attack live alone, with no immediate family member or spouse to turn to for physical and emotional support.
Tips for coping with depression
- A healthy lifestyle including regular exercise, proper sleep, a well-balanced diet, and relaxation and stress management techniques can help you manage depression.
- Engage in hobbies and activities you enjoy.
- Don’t use harmful habits to cope with your low mood, such as smoking, using drugs, drinking excessively, or overeating. These harmful habits increase your risk for heart disease and stroke.
- Get up and get dressed every day. A positive mood can lower blood pressure and give you the energy to focus on physical health and lowering the risk of cardiac events.
- The support and involvement of family and friends can be crucial in helping someone who is depressed. Make an extra effort to engage and socialize with friends and family.
- Because people with heart disease may have less energy and struggle with self-doubt it’s natural to withdraw and lose social confidence, making it harder to receive social support during difficult times. To help you cope and regain confidence ask your health care provider to recommend a psychotherapist or one of the many support groups for patients who have had heart surgery.
Heart disease and depression often have similar symptoms such as fatigue, low energy, difficulty in sleeping and carrying on the daily rhythms of life. Treating depression is as important as treating any other medical condition and when left untreated, depression can worsen heart disease and increase the risk of a heart attack.
References:
- Johns Hopkins Medicine:
- Cleveland Clinic:
https://my.clevelandclinic.org/health/diseases/16917-depression–heart-disease
- Harvard Health Medical School:
https://www.health.harvard.edu/heart-health/depression-and-heart-disease-a-two-way-street
- National Heart, Lung and Blood Institute:
https://www.nhlbi.nih.gov/news/2017/heart-disease-and-depression-two-way-relationship